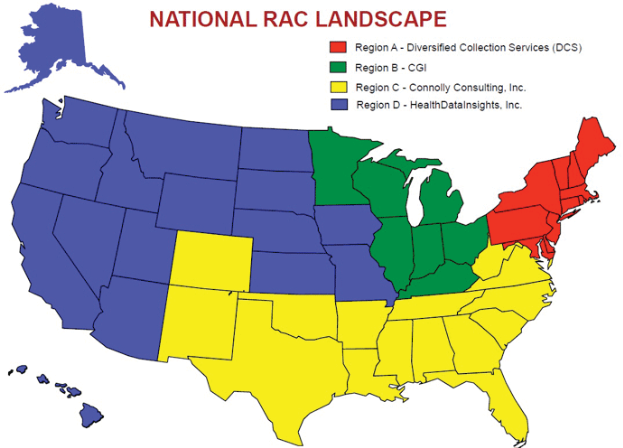
Recovery Audit Contractors
“RACs” are private companies that conduct post-pay audits of Medicare claims. They are paid, in part, based on the amount of improperly paid funds that they recover. The RAC demonstration project, enacted as part of the Medicare Modernization Act of 2003, was conducted between 2005 and 2008 in five States. It was a resounding success, identifying over $900 Million in overpayments while costing only a fraction of that amount. As a result of this success, in 2006, as part of the Tax Relief and Healthcare Act, Congress ordered the RAC program to be made permanent and expanded to all States. By 2010, all 50 States will have a RAC in operation. The RACs will begin provider/supplier reviews by looking for outliers, providers who have more than expected charges in a category. However there are NO limits on what they can look for, even if you have had a Medicare audit in the recent past, you may be targeted again.
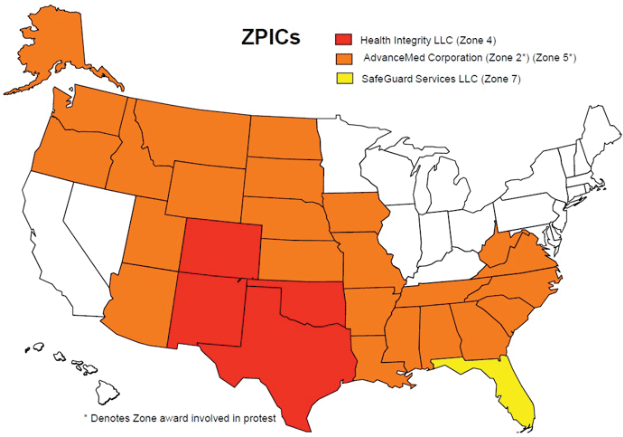
Program Safeguard Contractors
“PSCs” took over the traditional audit functions from the Carriers several years ago. The concept being that having the Carrier look for overpayments that they might themselves have created was not the best way to identify the overpaid funds. Thus, was born the independent PSCs. However many were merely spin-offs from the Carriers and not as independent or as aggressive as initially planned. With the new jurisdictions that are a part of the MACs, the PSCs are also being both re-aligned and reassigned. The new contractors will be called Zone Program Integrity Contractors (ZPICs), and, pursuant to CMS and OIG directives, they will be very active in reviewing data and conducting audits based on a small random sampling of your claims, generally from a two year time frame. CMS has made it clear that the RACs are not taking the place of the PSC/ZPICs. These two groups will be conducting audits independently of each other, the only limitation being that they will not review the same claims (but they may review the same provider/supplier).
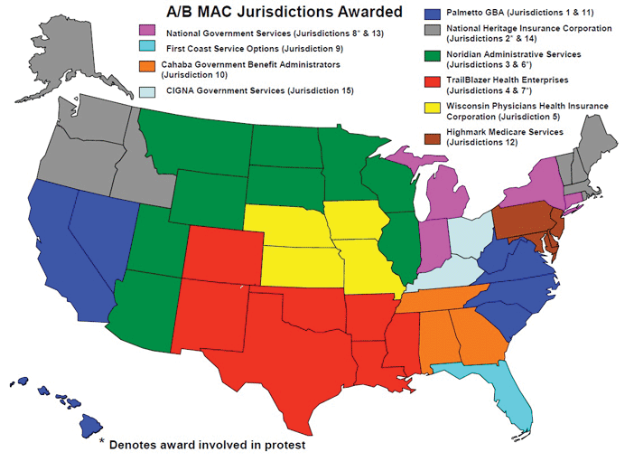
Medicare Administrative Contractors/Carriers
The RACs and PSCs/ZPICs are not the only eyes that will be looking for overpayments. The MACs will still have jurisdiction to review claims if their internal controls shows a pattern that is indicative of a possible overpayment. While the MACs do not have the same financial incentives to find overpayments that the RACs and PSCs do, they still have a responsibility to properly administer the program, and they will not want overpayments found by these other auditors to reflect poorly on their part. Therefore it is likely that they will continue to conduct probe reviews when prompted by their internal controls.
The OIG
The Office of Inspector General of the Department of Health and Human Services will also continue to conduct reviews of healthcare providers, which is their primary function. These investigations are usually initiated by an allegation of fraud or serious program abuse that comes to them from their fraud hotline or from any of CMS’s contractors (MACs, RACs, or ZPICs). In States where the OIG has investigated ambulance services in the past, we are seeing a continued focus on ambulance companies in those regions. It seems that once the OIG gets an understanding of issues that often arise in ambulance claims, they actively review other companies in their jurisdiction.
CMS
CMS's main office continues to conduct “CERT” reviews. These reviews are designed to collect data for industry-wide statistical purposes, however any claim that goes through CERT review may be referred to the MAC for recoupment or to the ZPIC or OIG if fraud or systemic abuse is suspected.
Medicaid Fraud Control Units
The Deficit Reduction Act made review of Medicaid payments mandatory for States that want to continue to receive Federal matching funds. Therefore, we are seeing many more Medicaid audits than we have in the past. Medicaid rules are often different than Medicare rules, and understanding those differences is very important. You must jump through the Medicaid specific hoops or risk an overpayment assessment in the event of an audit.